Precision-based treatment
1 in 26 people will develop epilepsy and the current “one size fits all model” is not effective for more than one third of patients who remain resistant to anti-seizure medications. Currently our anti-seizure medications do not treat the cause but rather just aim to reduce seizure burden.
What is the cause of my epilepsy?
The role of genomics has been well established in epilepsy, initially with family and twin studies and then with the discovery of single genes causing epilepsy. The importance of a genomic diagnosis is the great potential for targeted treatments, that can treat the cause.
Integrating genomic testing into clinical care
Genomics enables us to provide a better understanding of the cause of epilepsy for a particular patient. This approach will end the diagnostic odyssey of searching for how and why they developed epilepsy and will enable precision-based, personalised treatment approaches based on the individual’s genomic results.
How can my epilepsy be treated?
In vitro brain organoid drug screening platforms
Currently, finding the right medication can involve lengthy trials of sequential anti-seizure medications to get the most effective outcome for patients. Through the creation of a patient-specific (in vitro) epilepsy model and drug-screening platform, we can facilitate a new era of personalised, precision-based drug selection. This novel approach has the potential to change the current trial and error approach to get the right medication for patients more quickly.
Australian Institute for Bioengineering and Nanotechnology
Professor Ernst Wolvetang is an international leader in the field of pluripotent stem cell biology and functional genomics for almost 20 years. He is the senior group leader of the Stem Cell Engineering Group at The University of Queensland’s Australian Institute for Bioengineering and Nanotechnology (AIBN) and Co-director of the Centre for stem cell ageing and regenerative engineering (stemCARE).
Senior Group Leader, Head of the Stem Cell Engineering Laboratory
Email: e.wolvetang@uq.edu.au
Postdoctoral Research Fellow
Email: h.leeson@uq.edu.au
Postdoctoral Fellow
Email: s.pars@uq.edu.au
Postdoctoral Research Fellow in Organoid Biology
Email: m.shaker@uq.edu.au
Institute for Molecular Bioscience
We have collaborations with Professor Glenn King and his group, whose research harnesses the chemistry of venoms from arthropod predators, such as spiders, scorpions and centipedes, to develop novel pharmaceuticals to treat chronic pain, epilepsy and stroke. Current anti-seizure medications are suboptimal and have undesired side effects. Small peptides (proteins) from venoms are highly specific and effective but to date have not been tested in human cell types. We plan to test this new class of anti-seizure therapeutics in human brain and heart models and establish the requisite framework for first in human clinical trials in Australia.
Postdoctoral Research Fellow
Email: c.chow4@uq.edu.au
 Alexandra Sundman
Alexandra Sundman
PhD student
Email: a.sundman@uq.edu.au
Queensland Brain Institute
We have collaborations with Professor Helen Cooper and Associate Professor Tim Bredy from the Queensland Brain Institute. Associate Professor Tim Bredy is the Director of the Centre for RNA in Neuroscience . A primary objective of the Centre is to develop new tools to control RNA in the brain and design new RNA based therapeutics for the treatment of neurological disorders.
Visit the Centre for RNA in Neuroscience website
Deputy Director, QBI
Email: h.cooper@uq.edu.au
Director - Centre for RNA in Neuroscience, Group Leader, QBI
Email: t.bredy@uq.edu.au
Epilepsy Research Centre
We have a long and established collaboration with Professor Samuel Berkovic and Professor Ingrid Scheffer from the Epilepsy Research Institute in Melbourne. They are both clinician-researchers, who are international leaders in epilepsy genetics.
Laureate Professor in the Department of Medicine, University of Melbourne, and Director of the Epilepsy Research Centre at Austin Health
Monash University
We have established strong collaborations with Professor Terry O’Brien, Professor Patrick Kwan and Associate Professor Zongyuan Ge from Monash University, Melbourne. We have obtained a successful Medical Research Future Funds Stem Cell Missions Grant (2021-2024) in collaboration with Monash University. We have shared interests in using organoid models derived from a patient’s own cells to identify effective anti-seizure drugs in the dish and combining this with artificial intelligence, to identify effective drugs for patients faster and more precisely.
Chair of Medicine and Head, The Central Clinical School, Monash University
Program Director – Alfred Brain & Deputy Director of Research, Alfred Health
Chair, Australian Epilepsy Clinical Trials Network (AECTN)
Professor of Neurology in the Department of Neuroscience, Central Clinical School, Monash University
Consultant Neurologist and Director of the Epilepsy Unit at Alfred Health
 Associate Professor Zongyuan Ge
Associate Professor Zongyuan Ge
Monash Medical Artificial Intelligence Laboratory Director
Research Fellow, Department of Neuroscience
1. Spider venom peptides: precision therapy for genetic epilepsies
Current anti-seizure medications are suboptimal and have undesired side effects. Small peptides (proteins) from venoms are highly specific and effective but to date have not been tested in human cell types. Here we will test this new class of anti-seizure therapeutics in human brain and heart models and establish the requisite framework for first in human clinical trials in Australia.
2. Genomics and Epilepsy Clinical Outcomes (GECO)
Almost one third of epilepsy patients have to endure a “medication odyssey” in the hope of finding an effective treatment. To shorten or alleviate this burden, brain organoids can created from pluripotent stem cells derived from the blood cells of epilepsy patients that are drug responsive or drug refractory.
We next examine the brain organoid activity patterns to discover drugs and drug combinations that are effective in treating the drug resistant patients (using the responsive ones as controls). We envisage that this unique approach will dramatically shorten the “medication odyssey” that epilepsy patients have to endure without finding an effective treatment.
This project is in collaboration with Professor Ernst Wolvetang from The University of Queensland Australian Institute for Bioengineering and Nanotechnology.
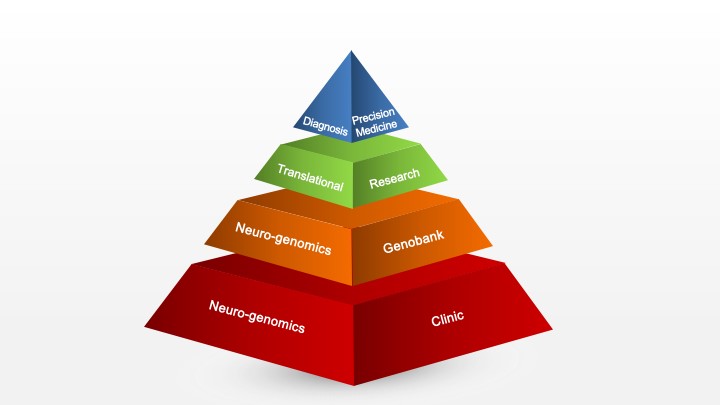
3. Developing a Queensland neuro-genomics service to underpin the era of precision-based medicine
To utilise genomic and neurological expertise to improve the diagnostic pathway and to facilitate precision-based management of patients with neurological conditions.
A neuro-genomics service supports the complex process of assessment, testing and return of results, in order to facilitate ongoing care for the individual and their family, in close conjunction with their treating neurologist. This genomic information will underpin the era of precision medicine, which holds great promise for treatment advances such as gene-specific therapy, where genomic information can be used to better treat or cure disorders.
We piloted a neurogenetics service for drug resistant epilepsy patients. The goal was to demonstrate that this model of care in drug resistant epilepsy patients will significantly improve their healthcare and show that this can be delivered using available resources effectively and efficiently.
4. Epilepsy Neurobiology of Anxiety, depression and Co-morbidities of Temporal lobe epilepsy (ENACT)
People with epilepsy are more likely than others to have mental health problems, including depression and anxiety, and people with depression and anxiety are more likely to develop epilepsy. This suggests that the underlying causes could overlap. The current treatment options for epilepsy and related mental health problems are limited and remain a challenge, so more research is needed to understand this better and develop new treatments.
The project will involve patients with temporal lobe epilepsy who are scheduled for epilepsy surgery as part of their treatment. The project uses blood samples and brain tissue that has been removed during surgery and donated for this research. Surveys will be used to measure depression and anxiety symptoms.
In this project, we will look at changes in cells and specific molecules in the brain tissue collected from patients with epilepsy. We are investigating if these changes are related to depression and anxiety symptoms.
Personalising Epilepsy Regimes with Stem cells and artificial Intelligence models for Superior Treatment outcomes (PERSIST)
This MRFF funded project will utilise cohorts of human induced pluripotent stem cell lines (hIPSC) derived from drug-responsive and drug-resistant epilepsy patients established across the two epilepsy research nodes (The University of Queensland and Monash University) and build on our collective expertise in generating hIPSC-derived brain organoids. We will also integrate our expertise in artificial intelligence models to further advance the algorithm.
We will use hiPSC-derived brain organoids and screen a library of approved drugs to identify those able to alter neural activity in a patient-specific model, train an artificial intelligence model that leverages both clinical and genomic data to assist drug selection, and validate treatment predictions in real-world clinical settings.
Demonstrating the utility of an epilepsy patient-specific in-vitro drug screening platform in combination with decision-making software offers substantive health benefits for patients, provides neurologists with an evidence-based medicine approach, reduces health care costs and has the potential to enable transformative new insights into the genetic drivers of epilepsy and drug-resistance, to inform new therapy development.
Channel 7: Spider venom could soon be used to help people living with drug-resistant genetic epilepsies - 8 September 2025Channel 10: Spider And Scorpion Venom Could Prevent Seizures In Epilepsy Patients - 8 September 2025Nine News Australia: How our creepy-crawlies are being used to save lives - 8 September 2025Nine News Australia: Spider venom hailed as potential epilepsy treatment - 8 September 2025




 Professor Glenn King
Professor Glenn King Dr Jonathan Chow
Dr Jonathan Chow